Cataract, Refractive, IOL
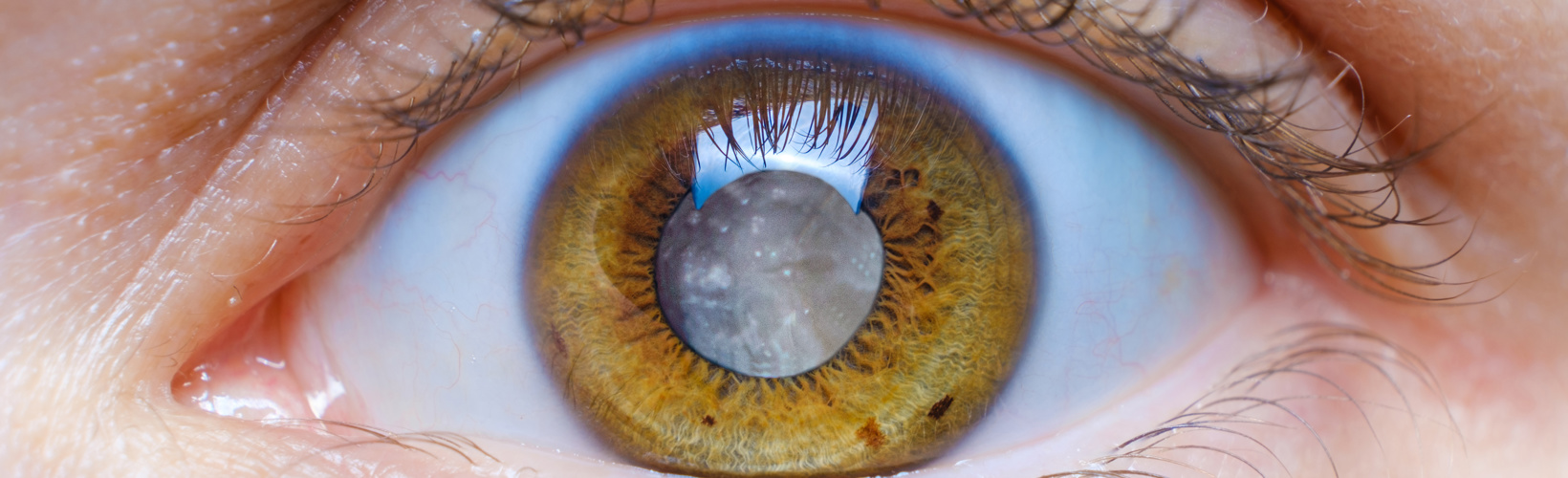
Capsulotomy in Intumescent White Cataract?
Experts express diverse opinions about the best technique.
Cheryl Guttman Krader
Published: Monday, September 2, 2024
Developments in surgical technologies for cataract surgery include new approaches for safely performing capsulotomy in eyes with an intumescent white cataract. Use of these tools, however, depends on access, patient characteristics, and surgeon comfort. Four leading cataract surgeons discussed their preferred technique for confronting these challenging cases.
Rengaraj Venkatesh MD advocated for manual capsulotomy performed with a double rhexis approach.
“There are many publications that establish how easily it can be performed,” he said, contrasting that benefit with the limitations of performing a femtosecond laser-assisted capsulotomy, precision pulse capsulotomy (PPC; Zepto), or selective laser capsulotomy (SLC; CAPSULaser).
Dr Venkatesh noted the femtosecond laser has a large footprint and requires additional staff for operation. Furthermore, the manually created capsulotomy has a smoother and stronger edge than the laser-created capsulotomy.
He said the potential for suction loss is a serious issue using PPC. Although there is evidence both PPC and SLC create a capsulotomy with a stronger edge than manual capsulotomy, Dr Venkatesh noted a lack of long-term data establishing whether the greater tensile strength offers benefit.
The added cost associated with using these automated devices could lead to patients compromising on their IOL choices.
“I think patients are better served having a procedure done by a premium surgeon with a manual capsulotomy and a premium IOL rather than a premium capsulotomy,” he said.
In favour of femtosecond laser
Nicole Fram MD discussed femtosecond laser-assisted capsulotomy. Describing it as “the easiest thing I have ever done to make a complex case routine,” she noted that problems with capsule friability encountered early on with femtosecond laser use have been overcome with new laser platforms containing more optimised settings to deliver less energy and friability of the anterior capsule. She also cited research showing better outcomes were achieved using the laser than a manual technique in shallow anterior chambers and brunescent cataracts.
However, a good outcome still depends on picking the right patient and following a proper docking protocol.
“We can make a complex case more routine using a femtosecond laser, but I think surgeons should consider a manual technique or a femtosecond laser-assisted mini capsulotomy if the anterior chamber is very shallow with a spheroidal appearance of the lens,” Dr Fram said.
Her tips for success using the femtosecond laser included staining the capsule with trypan blue, obtaining a very flat and well-centred dock, and completing the capsulotomy rapidly, ideally within 0.7–0.9 seconds. Dr Fram also suggested having an MST capsulorhexis forceps on hand for better control at capsulotomy completion. Often, an approach through a paracentesis will help avoid anterior chamber collapse and runout of the capsulotomy in an intumescent cataract, she said.
Precision pulse capsulotomy
For Vance Thompson MD, PPC represents the safest way to perform capsulotomy in eyes with an intumescent white cataract.
“The suction cup is easy to put on, and suction is reliably created when the device is connected to the phaco machine. The edge of the capsulotomy is very smooth and strong,” he said. “And one reason I think PPC is the best technology to use in white cataracts is it creates a 360-degree opening in just 0.4 milliseconds.”
In less advanced cataracts, Dr Thompson said he aligns the Purkinje 1 and 4 images for approximating patient fixation to centre the capsulotomy for 360 degrees of capsule overlap so the implant does not tilt or decentre with capsule contraction. He otherwise centres over the pupil in white cataract cases where Purkinje image-guided capsulotomy cannot be performed.
He noted the capsulotomy diameter usually turns out to be smaller in eyes with a white cataract than in those with less advanced cataracts because the capsule in eyes with an intumescent white cataract is under stretch. While he uses a capsule dye for intraoperative visualisation to avoid nicking the edge intraoperatively, he does not worry about creating tension on the capsule when dialling in a lens.
“We have shown in the laboratory that the capsule edge is quite strong with precision pulse technology,” he said.
Dr Thompson said he tends to avoid doing PPC in eyes with a deep anterior chamber (>3.8 mm) and those with a small pupil—although he noted other surgeons are comfortable using it in those situations.
Selective laser capsulotomy
Richard Packard MD favours SLC in cases of intumescent white cataract.
“The laser has been used in over 20,000 eyes, and none with an intumescent cataract had an Argentinian flag sign,” he said.
Summing up the main reasons for his preference, Dr Packard stated, “The selective laser creates a capsulotomy of consistent size, consistent circularity, and a strong elastic edge in less than 0.3 seconds. Not only does the capsulotomy give 360-degree coverage of the IOL, but the coverage is symmetrical, which is very important for premium and capsulotomy-fixated IOLs.”
The 590 nm laser beam is absorbed selectively by a capsule stained with a microfiltered 0.4% trypan blue solution. Patient fixation is not normally possible with an intumescent cataract, thus making the visual axis—and centration—difficult to determine. The SLC technique overcomes this issue, Dr Packard said.
“Centration on the visual axis is aided by having an area of enhanced staining within the capsule centre coincident with the first and fourth Purkinje reflex,” he explained.
To overcome intralenticular pressure, Dr Packard overfills the anterior chamber with a high molecular weight ophthalmic viscosurgical device to flatten the anterior capsule.
Drs Venkatesh, Fram, Thompson, and Packard spoke at ASCRS 2024 in Boston, US.
Rengaraj Venkatesh MD is the Chief Medical Officer of Aravind Eye Hospital, Pondicherry, India. venkatesh@aravind.org
Nicole R Fram MD is the managing partner at Advanced Vision Care, Los Angeles, US. nicfram@yahoo.com
Vance Thompson MD is the director of refractive surgery at Vance Thompson Vision, Sioux Falls, South Dakota, US. vance.thompson@thompsonvision.com
Richard Packard MD is a senior consultant at Arnott Eye Associates, London, UK. eyequack@vossnet.co.uk
Tags: SLC, selective laser capsulotomy, capsulotomy, Rengaraj Venkatesh, Nicole R Fram, Vance Thompson, Richard Packard, IOL, cataract surgery, intumescent, intumescent cataract, PPC, precision pulse capsulotomy, femtosecond laser, femto laser, premium IOLs, double rhexis
Latest Articles
Towards a Unified IOL Classification
The new IOL functional classification needs a strong and unified effort from surgeons, societies, and industry.
Organising for Success
Professional and personal goals drive practice ownership and operational choices.
Update on Astigmatism Analysis
Is Frugal Innovation Possible in Ophthalmology?
Improving access through financially and environmentally sustainable innovation.
iNovation Innovators Den Boosts Eye Care Pioneers
New ideas and industry, colleague, and funding contacts among the benefits.
José Güell: Trends in Cornea Treatment
Endothelial damage, cellular treatments, human tissue, and infections are key concerns on the horizon.
Making IOLs a More Personal Choice
Surgeons may prefer some IOLs for their patients, but what about for themselves?
Need to Know: Higher-Order Aberrations and Polynomials
This first instalment in a tutorial series will discuss more on the measurement and clinical implications of HOAs.
Never Go In Blind
Novel ophthalmic block simulator promises higher rates of confidence and competence in trainees.